Knowledge Mobilisation & Academic Career Development
What is knowledge mobilisation (KM)?
NIHR defines it as:
"Getting the right information to the right people in the right format at the right time, so as to influence decision-making. Knowledge Mobilisation includes dissemination, knowledge transfer and knowledge translation."
A central feature of KM is democratisation of knowledge.
Our HPRU KM Lead and Strategy
Lead: Dr Raheelah Ahmad
Strategy:
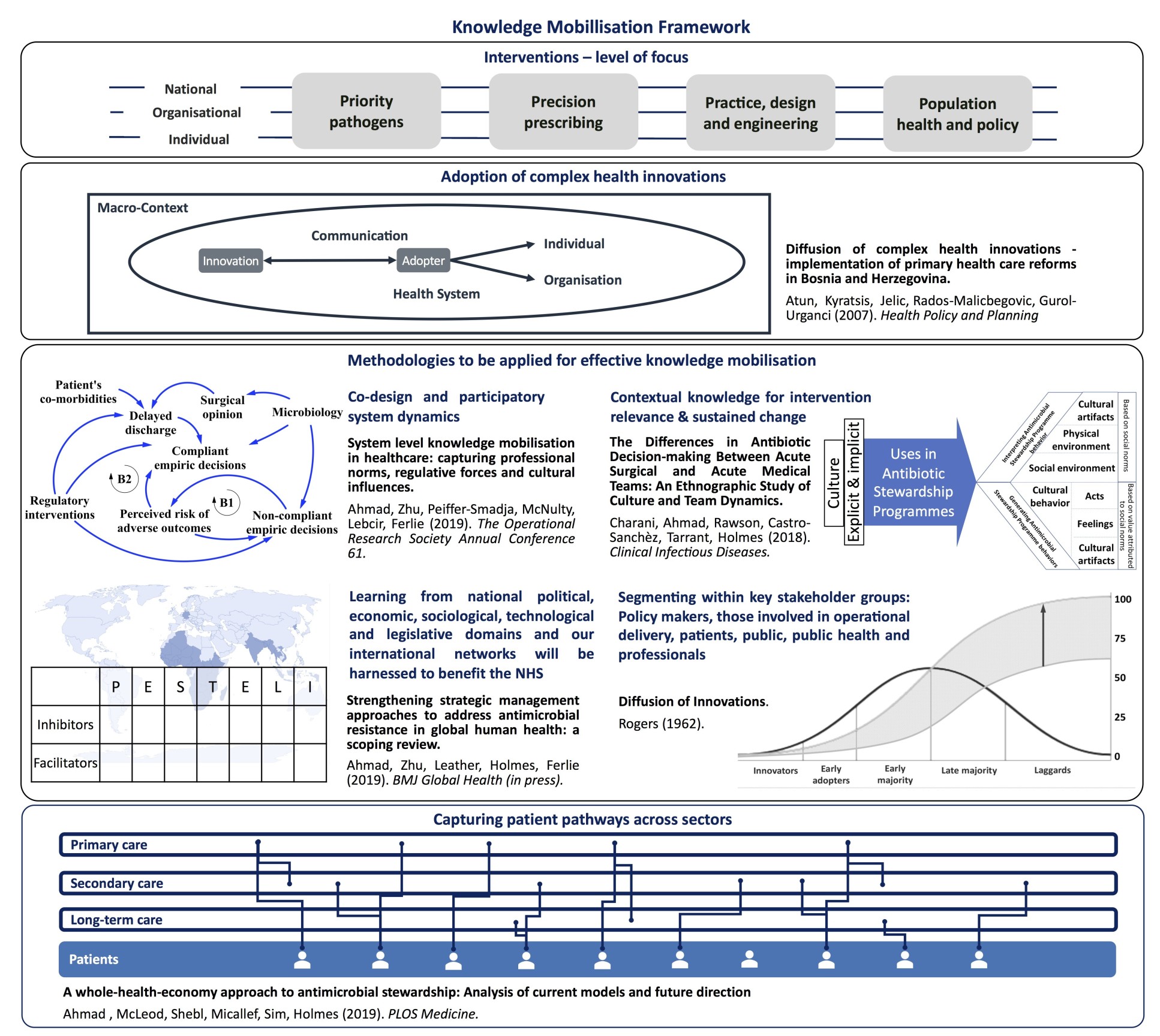
Having developed an enhanced and systematic approach for early stakeholder engagement to optimise KM, collaborators spanning primary, acute and long-term care providers in London, South/South-East of England, the third sector, policy makers, and all relevant sections within UK-HSA, will collectively analyse the environmental domains facilitating uptake of scientific evidence and other outputs. Learning from national political, economic, sociological, technological and legislative domains and our international networks will be harnessed to benefit the NHS (see figure).
‘Ground-up’ workshops (HPRU team, NHS operational delivery staff, PPI reps) will complement this macro-level analysis to draft a Theory of Change (ToC) setting out assumptions, preconditions, interim steps and outcomes needed to reach the impact identified in the strategic plan. Our management committee will consider the ToC to ensure consistency with the overarching strategic format and thereafter a ‘live’ document reviewed by theme leads/teams quarterly, the committee twice yearly, and validated by the Advisory Board annually.
We will exploit the novel participatory system dynamics simulation methodology to (a) leverage existing data, literature, expert knowledge, and behavioural variables, allowing a transparent, low-risk/low-cost simulation of impact of policy and service delivery options and (b) enhance organisational learning and mental models of different stakeholders. The methodology recognises that KM in healthcare is nonlinear, driven by multi-sectoral stakeholders, and can be highly reactive, i.e. in patient-GP interactions, or slow and highly protracted, i.e. in technology adoption.
As well as strategic oversight, our lead will have operational responsibility for
- facilitating ToC workshops informed by our work on sustained change and culture;
- ensuring best KM practice is scaled up within and between the Imperial HPRUs;
- organising learning exchange with the Oxford HPRU on AMR and HCAIs;
- aligning outputs to coordinate Patient Participation, Involvement and Engagement in research and NIHR research dissemination;
- sourcing/delivery of capacity building jointly with The Forum; and
- agreeing with the HPRU Directors, agenda and scientific papers for discussion at the successor to the Patient Safety All-Party Parliamentary Group, for which our Faculty of Medicine will serve as secretariat.
WAAW2020 webinar: United to Preserve Antimicrobials
Our existing ethos is that tackling AMR and HCAI requires a multidisciplinary and multi-professional workforce. This is reflected in our track-record of attracting and developing bench-scientists, epidemiologists, doctors, nurses and those from under-represented professions such as pharmacists. The unique environment and infrastructure of the HPRU provides opportunities for researchers and Trust staff to work closely and we have supported fellowship applications from NHS Managers, Doctors, Nurses, Pharmacists and Healthcare Scientists, to develop proposals which address service challenges. We recognise the importance of all these professions in directing and developing translational research and in particular will continue to support Healthcare Scientist roles, career progression and the local Training programme. This strategy aligns closely with the NIHR Academy and its encouragement of collaborative, multi-professional research.
Internally we have established local methodological training in quantitative, qualitative and behavioural sciences to support our mixed methods approach and arranged bespoke PPI/E/P training for staff. Vibrant peer-to-peer meetings and an extensive range of training opportunities offered through the College Graduate School, Postdoc and Fellows Development Centres and the Staff Learning and Development Centre, helps foster a respect for the diversity of methodological and theoretical practices which is core to the NIHR Academy.
One of our key objectives has been to retain staff and students that the HPRU has invested in, and to support them to the next career stage. We believe this proactive approach has the dual benefit of preserving newly developed expertise in shortage areas and addressing at least some of the causes for high attrition rates amongst postdocs, particularly women. Our ambition for this HPRU is to maintain our core of as many of our experienced staff as possible, giving them increased responsibility for independently managing the research within themes supported by our senior research Theme Leads and HPRU dedicated administrative support. We aim to see some of them progress to academic positions during the life of the award, following the route for career progression which we have established.
In tandem, we will train the next cohort of public health researchers through the development of 4 new PhD students.
Our named training lead Prof Sriskandan is Clinical Training Director for the MRC Centre for Molecular Bacteriology and Infection and NIHR ACF Clinical Academic Training-Lead for ID/Microbiology at Imperial. We have close ties with the Imperial Clinical Academic Training Office (CATO).
CATO, under the leadership of Professor Jeremy Levy, is a centralised pan-professional academic training hub and point of contact for advice and information on academic careers. The CATO ensures that clinical academic trainees of any professional background (doctors, nurses, physiotherapists, dieticians etc) have mentoring, academic guidance, access to the Imperial College Graduate School and Post-Doctoral and Fellows Development Centre for professional development, a generic multiprofessional Masterclass programme (e.g. ‘How to interact with journalists and the public’; “Health economic evaluations for researchers”; “pitfalls in using Big Data”), a non-medical researcher development programme and internal research presentations, symposia and support for fellowship applications, and benefit from cohorting, and an annual interprofessional and specialty research conference.