Contact us
For any enquiries related to Microvesicles in Acute Respiratory Distress Syndrome, please contact
Dr Sanooj Soni
s.soni@imperial.ac.uk
What we do
We investigate the propagation of lung injury and in critically unwell patients and peri-operative patients. This has predominantly focused upon the role of microvesicles in acute respiratory distress syndrome (ARDS). Our group is primarily interested in cellular communication and the transfer of inflammatory cargo/milieu between alveolar and pulmonary cells during lung injury as well as pulmonary cells to peripheral organs. We are also currently exploring the role of MVs in COVID-19 induced ARDS and multi-organ failure.
Why it is important
ARDS
Patients with ARDS have a high mortality and consume considerable healthcare resources due to severity of illness and long intensive care stays. Despite intense research, there are no disease modifying therapies for ARDS. There remains an urgent, unmet need for a re-direction in ALI research to identify novel therapeutic targets, which may lead to new treatments.
Perioperative
Each year, over 310 million major surgical cases are performed worldwide with 2.4 million general anaesthetics administered in the UK alone. Postoperative pulmonary complications (PPCs) occur in up to 33% of cases, significantly increasing short- and long-term mortality and morbidity, and hospital length of hospital stay with its attendant costs. Among various potential causes of PPCs, mechanical ventilation, used during peri- and/or post-operative period with major surgery, is a major contributing factor, as it often produces unphysiological alveolar stretch instigating lung inflammation and injury, a pathophysiology termed as ventilator-induced lung injury (VILI). Our understanding of the mechanisms underpinning the pathophysiology of VILI is still primitive resulting in a lack of effective treatments and subsequent poor outcomes.
COVID-19
A significant proportion of hospitalised patients with COVID-19 require intensive care due to ARDS (ARDS) and multi-organ failure (MOF). Indeed, 51.8% COVID-19 ARDS patients develop acute kidney injury (AKI), which has a mortality of 61%. Management remains principally supportive and there remains an urgent need for research investigating mechanisms of respiratory/kidney failure in COVID-19 to identify novel diagnostic/therapeutic targets.
Funders and collaborators
There is an urgent and compelling need to better understand the fundamental mechanisms of ARDS and associated MOF in both ICU and perioperative patients, to identify targets from entirely novel perspectives, which allow development of more specific and effective therapies. We hypothesise that MVs, released within the lungs and into the circulation, play crucial roles in the evolution of ARDS as well as in transmitting inflammation to peripheral organs, producing AKI/MOF.
By investigating the previously un-tested body compartment "extracellular MVs", we will identify a novel alternative inflammatory pathway/target that is closely linked with key pathophysiology of ARDS/MOF, to aid diagnosis, phenotype differentiation, prognostication and treatment personalisation.
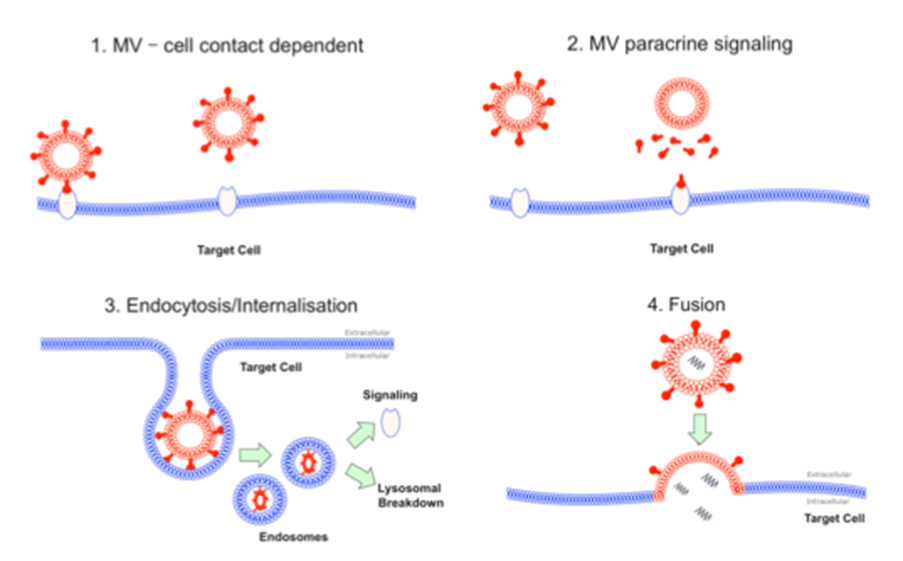
Most recently, we have demonstrated a dynamic production of MVs from multiple intra-alveolar cells early in the inflammatory course of acute lung injury (ALI) particularly from alveolar macrophages. When instilled into murine lungs, these MVs induced lung injury via a TNF dependent mechanism. We found that TNF is released within MVs via an unconventional endoplasmic reticulum/Golgi-independent route (similar to IL-1β), despite being a classical, golgi-dependant cytokine. Interestingly, we demonstrated that this switch in cellular TNF trafficking is mediated via acid sphingomyelinase.
We also characterised MV populations within bronchoalveolar lavage taken from COPD patients and found that neutrophil-derived MVs strongly correlated with disease severity. We have similarly characterised MVs populations in bronchoalveolar lavage fluid taken from patients post lung tranplantation with Primary Graft Dysfunction (PGD) and in patients with ARDS.
Currently we are also running a large multi-centre clinical translational study ’multi-organ failure in SARS-CoV-2: identifying mechanisms and potential therapeutic targets’.
Funders
Koh MW, Baldi RF, Soni S, Handslip R, Tan YY, O'Dea KP, Malesevic M, McAuley DF, O'Kane CM, Patel BV, Takata M, Wilson MR. Secreted Extracellular Cyclophilin A is a Novel Mediator of Ventilator Induced Lung Injury. Am J Respir Crit Care Med. 2021 Apr 13. doi: 10.1164/rccm.202009-3545OC.
Soni S, Garner J, O;dea K, Koh, M, Tirlapur N, Srikanthan K, Tenda R, Faelkady A, Singh S, Wilson MR, Kemp S, Usmani O, Shah P, Takata M. Intra-alveolar neutrophil-derived microvesicles are associated with disease severity in COPD. Am J Physiol Lung Cell Mol Physiol. 2021 Jan 1;320(1): L73-L83.
Chia G, Barrett H, Patel P, Soni S. One hundred eighteen days on a ventilator: a COVID-19 success story against all odds. BMJ Case Rep. 2021 Mar 29;14(3):e239631.
Chaggar RS, Shah SV, Berry M, Saini R, Soni S, Vaughan D. The Video Classification of Intubation (VCI) score: a new description tool for tracheal intubation using videolaryngoscopy: A pilot study. Eur J Anaesthesiol. 2021 Mar 1;38(3):324-326.
Stephens JR, Wong JLC, Broomhead R, Stümpfle R, Waheed U, Patel P, Brett SJ, Soni S. Raised serum amylase in patients with COVID-19 may not be associated with pancreatitis. Br J Surg. 2021 Apr 30;108(4):e152-e153.
Gasparini M, Khan S, Patel J, Parekh D, Bangash M, Stumpfle R, Shah A, Baharlo B and Soni S. Renal impairment and its impact on clinical outcomes in critically ill patients with COVID-19: a UK multicentre observational study. Anaesthesia 2021.
Stephens J, Stumpfle R, Patel P, Brett S, Broomhead R, Baharlo B and Soni S. Analysis of critical care severity of illness scoring systems in patients with COVID-19: a retrospective analysis of three UK intensive care units. Crit Care Med 2021.
Soni S, Shah S, Chaggar R, Saini R, James E, Elliot J, Stephens J, McCormack T, Hartle A. Surgical cancellation rates due to peri-operative hypertension: Implementation of multi-disciplinary guidelines across primary and secondary care. Anaesthesia 2020;75(10):1314-1320
O'Dea KP, Tan YY, Shah S, V Patel B, C Tatham K, Wilson MR, Soni S, Takata M. Monocytes mediate homing of circulating microvesicles to the pulmonary vasculature during low grade systemic inflammation. Journal of extracellular vesicles. 2020; 5;9(1):1706708 2nd senior author
Soni S, Tirlapur N, O'Dea KP, Takata M, Wilson MR. Microvesicles as new therapeutic targets for the treatment of the acute respiratory distress syndrome (ARDS). Expert Opin Ther Targets. 2019;23(11):931-941
Oakley C, Koh M, Baldi R, Soni S, O'Dea K, Takata M, Wilson M. Ventilation following established ARDS: a preclinical model framework to improve predictive power. Thorax. 2019;74(12):1120-1129.
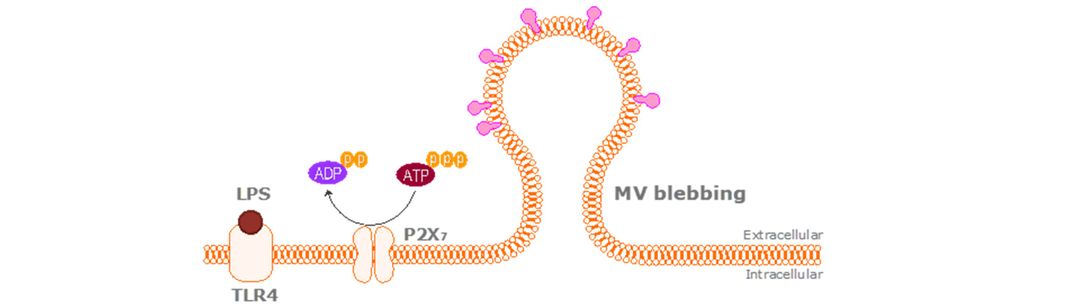
Soni S, O'Dea KP, Tan YY, Cho K, Abe E, Romano R, Cui J, Ma D, Sarathchandra P, Wilson MR, Takata M. Danger signals redirect cytokine trafficking and promote novel membrane TNF signalling via microvesicles. FASEB J. 2019:fj201802386R.
Soni S, Wilson MR, O'Dea KP, Yoshida M, Katbeh U, Woods SJ, Takata M. Alveolar macrophage-derived microvesicles mediate acute lung injury. Thorax. 2016 Nov;71(11):1020-1029.
Researchers
Dr Sanooj Soni
/prod01/channel_3/media/images/people-list/Sanooj-Soni.jpeg)
Dr Sanooj Soni
Professor Masao Takata
/prod01/channel_3/media/images/people-list/Professor-Masao-Takata.jpeg)
Professor Masao Takata
Dr Michael Wilson
/prod01/channel_3/media/images/people-list/Dr-M-Wilson.jpg)
Dr Michael Wilson
Dr Kieran O'Dea
/prod01/channel_3/media/images/people-list/K-O'dea-(1).jpg)
Dr Kieran O'Dea
Dr Yoichi Iki
/prod01/channel_3/media/images/people-list/No-Pic-portrait-reformated.jpg)
Dr Yoichi Iki
Miss Dane Cheng
/prod01/channel_3/media/images/people-list/No-Pic-portrait-reformated.jpg)
Miss Dane Cheng
Miss Sehar Khushi
/prod01/channel_3/media/images/people-list/No-Pic-portrait-reformated.jpg)
Miss Sehar Khushi
PhD students
Dr Jonathan Stevens
/prod01/channel_3/media/images/people-list/No-Pic-portrait-reformated.jpg)
Dr Jonathan Stevens
Miss Diane Cheng
/prod01/channel_3/media/images/people-list/No-Pic-portrait-reformated.jpg)
Miss Diane Cheng