What we do
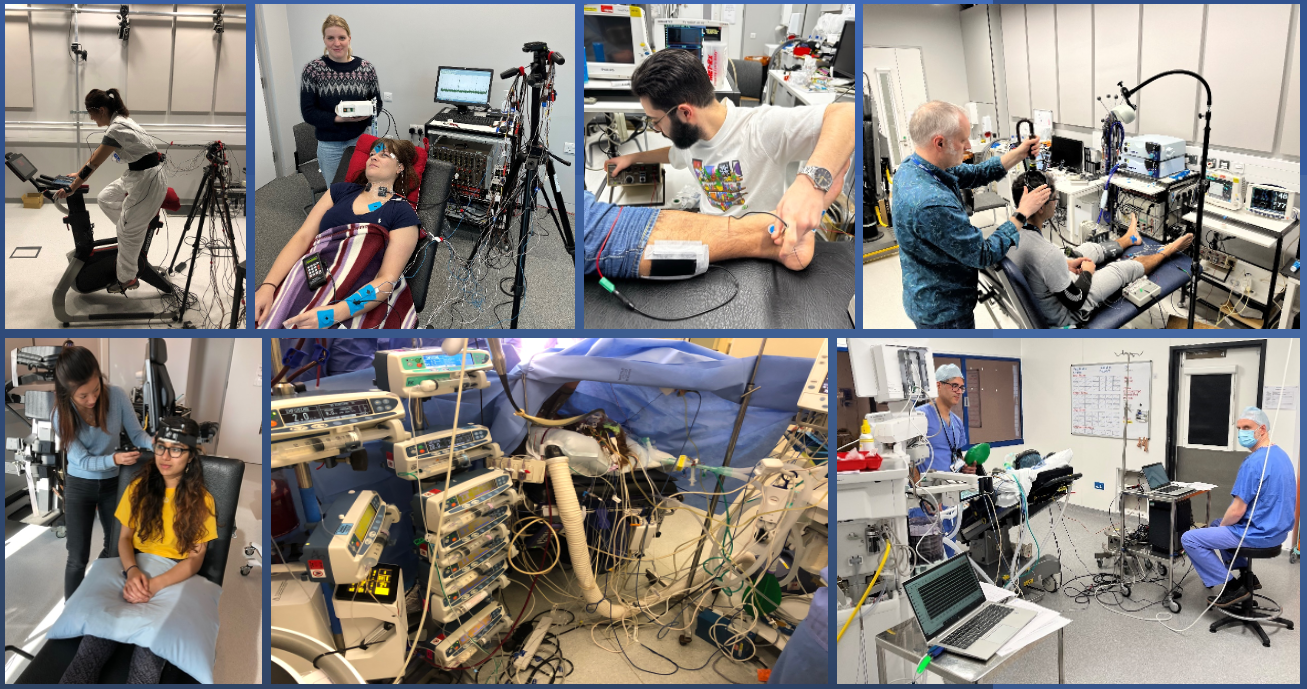
Our research aims to gain new insights by creating models of clinical scenarios in the laboratory and by setting up “field” laboratories in clinical settings. We use our expertise in applied physiology and neurophysiology research methods to tackle a diverse range of research questions that are linked by their relevance to anaesthesia, perioperative medicine, and those who deliver it.
Why it is important
Whole human physiology is a method of bridging the translational gap. Models and interventions that work at a cellular or sub-cellular level do not necessarily translate into solutions that work in the real world for patients. Whole human physiology can interrogate such models and interventions in healthy humans and patients and thus facilitate the development of real-world solutions.
How it can benefit patients
Our research has benefits, not only for patients, but also for healthy populations, such as healthcare workers. The range of benefits matches the diversity of research questions but can be summarised as increasing understanding of physiological and disease mechanisms, and the development of novel diagnostic and therapeutic interventions.
Summary of current research
Humans can tolerate a narrow range of body temperatures. Both hypo- and hyperthermia have potentially life-threatening consequences. As global temperatures rise, heat illness is an increasing concern. We are investigating the mechanism and consequences of epidural hyperthermia, and the impact of personal protective equipment (PPE) use on healthcare workers.
Epidural hyperthermia occurs during 20% of labour epidurals and has a negative impact on both the mother and baby. With the support of the Obstetric Anaesthetists’ Association and Imperial Healthcare Charity, we are investigating the “sympathetic blockade” mechanism; the impact upon neonatal neurological outcome; and the efficacy of a potential solutions.
Use of Personal Protective Equipment (PPE) has increased in healthcare during the COVID-19 pandemic in order to prevent disease transmission. Its use has clear benefits, but it can also cause heat illness in those who wear it. With the support of the BMA foundation, we are investigating the impact of airborne PPE on healthcare workers performance and wellbeing.
Anaesthesia is mediated through the effects of drugs on the central and peripheral nervous systems. Neurophysiology is a means of quantifying these effects. We are employing neurophysiological methodologies to investigate the concept of patient controlled inhalational sedation and are developing methods of detecting spinal cord injury during vascular surgery.
Use of sedation, rather than general anaesthesia, has benefits for patients, clinicians and healthcare organisations. However, clinician delivered sedation is underutilised, due to concerns about safety and intraoperative awareness. Patient controlled sedation is a potentially superior alternative, but little is known about this technique. Therefore, we are working with Intersurgical Ltd to gain a greater understanding of its safety and efficacy.
The risk of spinal cord injury following endovascular aortic aneurysm repair is up to 10%. Increasingly, spinal cord injury is seen post-operatively, limiting the use of current monitoring modalities. If damage to the spinal cord can be detected perioperatively, strategies can be employed to mitigate it. Therefore, we are investigating the efficacy of transcranial magnetic stimulation and near infrared spectroscopy to detect spinal cord injury in the perioperative period.
Information
Chaudhari N, Strutton PH, Wickham AJ, McGregor AJ, Mullington CJ. Heat stress associated with aerosol PPE and its impact. Occupational Medicine 2022 [online ahead of print].
Gimzewska, M; Berthelot, M; Sarai, P; Geoghegan, L; Onida, S; Strutton, PH; Shalhoub, J; Davies, AH. Evaluation of a novel wireless near infrared spectroscopy (NIRS) device in the detection of tourniquet induced ischaemia. BMJ Innovations2022; 8(1).
Morton, S; Kua, J; Mullington, CJ. A Systematic Review and Meta-Analysis of Epidural Analgesia, Intrapartum Hyperthermia and Neonatal Brain Injury. BJA 2021; 126(2):500-515.
Mullington, CJ; Malhotra, S. Hyperthermia after epidural analgesia in obstetrics. BJA Ed 2021; 21(1):26-31.
Mullington, CJ; Low, DA; Strutton, P; Malhotra, S. A mechanistic study of the tremor associated with epidural anaesthesia for intrapartum caesarean delivery. IJOA 2020; 43:56-64.
Mullington, CJ; Low, DA; Strutton, P; Malhotra, S. Body temperature, cutaneous heat loss and skin blood flow during epidural anaesthesia for emergency caesarean section. Anaesthesia 2018; 73(12):1500-1506.
Sarai, P; Bicknell, C; Courtois, N; Strutton, PH. Can Transcranial Magnetic Stimulation be used to detect potential spinal cord injury following thoracic endovascular aortic repair (TEVAR)? A preliminary study to characterise baseline motor evoked potentials in vascular disease patients. European Journal of Vascular and Endovascular Surgery 2018. 56(6):e30.
Researchers
Dr Chris Mullington
/prod01/channel_3/media/images/non-standard-dimensions/chris-M.jpeg)
Dr Chris Mullington
Honorary Clinical Senior Lecturer
Dr Pav Sarai
/prod01/channel_3/media/images/people-list/106EDE36-6988-41DA-9088-1F61EF5B6479.jpeg)
Dr Pav Sarai
Honorary Clinical Senior Lecturer