
What we do
We take a clinical translational approach to elucidate novel physiological and biological mechanisms of organ failure during critical illness, with the ultimate aim of improving the management and outcomes of patients admitted to critical care. We take clinically relevant observations and ask how they could be investigated further using experimental medicine approaches leading to novel understanding and future treatments.
The group focuses on advanced heart and lung failure especially those supported on extracorporeal technologies.

Our research
Critical illness is a state and critical care is an area in a hospital. patients fulfilling both are often defined by being on a ventilator or requiring multi-organ support. Whilst mechanical ventilation saves lives through supporting gas exchange, it can also lead to significant harm, and being in critical care for prolonged periods (chronic critical illness) exposes patients to other effects such as chronic organ dysfunction e.g. lung fibrosis, delirium, ICU acquired muscle wasting, all of which have life altering consequences.
Our aim is to understand pinch points in care such that patients can be discharged from ICU appropriately earlier but also avoiding these longer term consequences. Patients requiring advanced critical care support are an example where these consequences occur more frequently and our vision is to better understand the clinical, biological and physiological trajectories and pathways that patients are exposed to, but also apply novel technologies at different stages to improve patient outcomes.
Clinical informatics analyses
COVID-ICU: National Service Evaluation.
- https://www.imperial.ac.uk/artificial-intelligence/research/covid/covidicu/
- https://www.thelancet.com/journals/lanres/article/PIIS2213-2600(21)00317-9/fulltext?rss=yes
- https://www.esicm.org/esicm-talk-episode-8-what-happened-mechanically-ventilated-covid19-patients-uk/
- https://www.rbht.nhs.uk/news/artificial-intelligence-predicts-best-treatment-for-covid-19-patients
Ventilatory Clinical Decision Support
Open-Loop Weaning Algorithm for mechanical VEntilation: comparison of open-loop decision support system versus routine care in cardiothoracic patients. The WAVE study.
ECMO-BIOMARKER – Personalised physiological and biological approach to ARDS management
- https://www.imperial.ac.uk/news/193590/25-million-eu-grant-help-save/
- https://www.bbc.co.uk/news/av/uk-england-london-50323592
- https://www.standard.co.uk/news/london/25m-trial-of-ai-system-to-help-patients-at-risk-of-fatal-lung-failure-a4268761.html
- https://www.imperial.ac.uk/news/199975/trial-explore-more-effective-treatments-seriously/
- https://www.imperial.ac.uk/news/200433/imperial-researchers-inform-smarter-regulation-healthcare/
Understanding human-machine interface in extracorporeal circuits
Haemostasis and Immuno-Thrombosis in Extracorporeal Circuits (The HITEC study).
Understanding pulmonary immune responses during severe acute respiratory failure
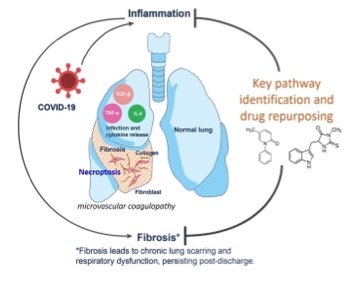
Mechanisms of dysregulated pulmonary fibrosis in ARDS: opportunities for drug repurposing in COVID-19.
Neutrophil – endothelial necroptotic interactions and the propagation of inflammation.
Therapeutic targeting of necroptosis cell death pathways in COVID-19 ARDS: proof-of-principle.
Cell death programmes in the persistence and resolution of clinical ARDS.
Clinical trajectory and mechanisms in ICU acquired weakness.
Research repurposed for COVID-19:
- Blood-thinning drugs can help save Covid-19 patients' lives
- Clear link” between COVID-19 and blood clotting – UK research team - Article no longer available
- Trust research shows link between blood vessel disease and severe COVID-19
- Trust researchers at forefront of COVID-19 research
- Supporting global research efforts for COVID-19
AJRCCM publication highlighted in Blue Briefings:
- Blue Briefing: Pulmonary Angiopathy in COVID-19 - Physiologic, Imaging and Hematologic Observations
- Portraits of NHS staff at the Royal Brompton Hospital, Chelsea
- Imperial AHSC Covid-19 webinar
- Imperial AHSC Lung Injury and Critical Care webinar
- How your donations helped our staff during the COVID-19 outbreak
- COVID-19 Response Fund: new projects advance the fight against coronavirus
Information
Funders
- European Commission
- National Institute for Health Research
- Royal Brompton and Harefield Charity
- EuroELSO
- Imperial College Covid-19 response fund
- HCA Clinical fellowships – Wellington Hospital, London
Industry links
- Mermaid A/C, Denmark
Internal
- Prof Ian Adcock, NHLI, ICL
- Dr Phil Molyneaux, NHLI, ICL
- Prof Aldo Faisal, Faculty of Engineering, ICL
- Dr Yap Choon, Faculty of Engineering, ICL
External
- Prof Danny McAuley, Queens University, Belfast, UK
- Prof Stephen Rees, Aalborg University, Denmark
- Dr Zudin Puthocheary, QMUL, UK
- Dr John Prowle, QMUL, UK
- Prof Stephen Harridge, King’s College London, UK
- Dr Luigi Camporota, King’s College London, UK
Researchers
Dr Brijesh Patel
/prod01/channel_3/media/images/people-list/Patel_Brijesh.jpeg)
Dr Brijesh Patel
Clinical Senior Lecturer in Cardiothoracic
Dr Kieran O’Dea
/prod01/channel_3/media/images/people-list/K-O'dea-(1).jpg)
Dr Kieran O’Dea
Senior Lecturer in Translational Critical Care
Dr Sharon Mumby
/prod01/channel_3/media/images/people-list/Holding-PNG--tojpeg_1564655919889_x2.jpg)
Dr Sharon Mumby
Research Associate
PhD Students
Dr Rhodri Handslip
/prod01/channel_3/media/images/people-list/Holding-PNG--tojpeg_1564655919889_x2.jpg)
Dr Rhodri Handslip
Research Postgraduate